
Optimize ABA Session Notes with our comprehensive guide, streamlining documentation for RBTs and BCBAs.

By Joshua Napilay on Sep 02, 2024.
Fact Checked by RJ Gumban.

Applied behavior analysis (ABA) therapy aims to improve behaviors, enhance learning, and reduce challenging behaviors in individuals, especially children with autism spectrum disorder. It uses methods such as discrete trial training (DTT) to teach skills in small steps systematically and a picture exchange communication system (PECS) to aid non-verbal communication through picture cards.
During ABA therapy, ABA Session Notes record individuals' behavior and progress. They are written by registered behavior technicians (RBT) or board-certified behavior analysts (BCBA).
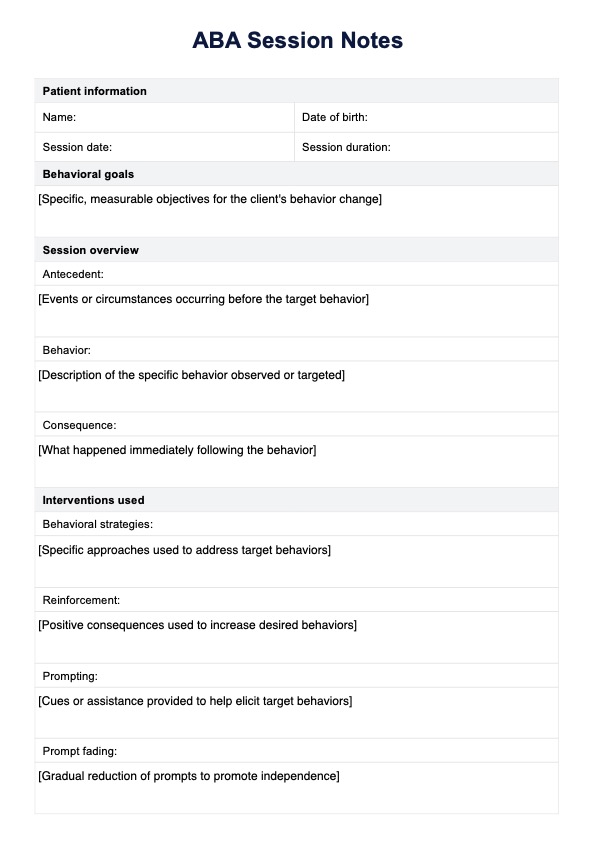
An ABA session note typically includes the following information:
To ensure accuracy and transparency, you should write session notes immediately so the details remain fresh. If you want a general template that fits into your practice, the Session Notes Template is a handy tool. You can also use ABA SOAP notes for a more structured way of documenting progress notes. Our SOAP Notes for ABA Therapy Template can be a helpful resource for this.
PDF Template Example PDF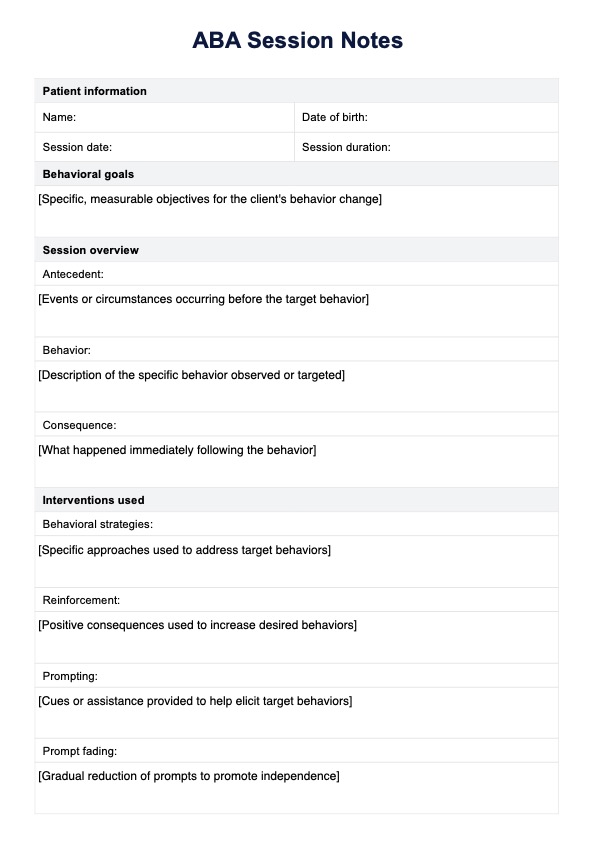
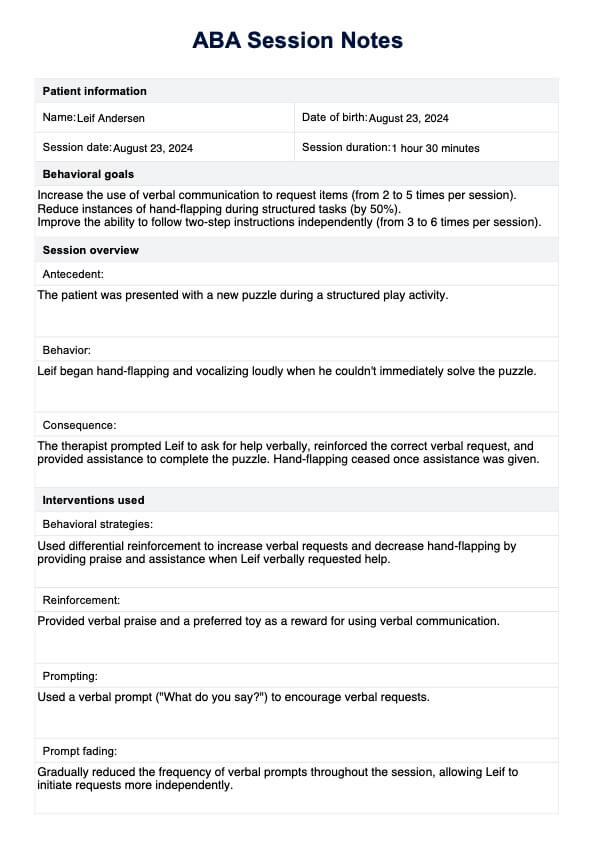
Writing concise ABA notes completes a client's therapy session. These notes provide a comprehensive view of the client's progress, including measurable and observable data, behavior targets, and intervention responses. Here are some simple steps to follow to use our template:
First, download the ABA Session Notes template to your computer or device.
Enter the patient's name, birthdate, session date, and how long the session lasted. This information keeps records organized and helps track progress over time.
Define the specific goals for the session and describe how you plan to achieve them. This includes explaining the strategies and methods used during the session to address behaviors.
Record data on the behaviors observed during the session. This includes how often each behavior occurred, how long they lasted, and their intensity.
Assess how well the patient is progressing towards their goals. Based on what you observed during the session, note any strengths they showed and areas where they can improve.
Document any communication with caregivers or other professionals involved in the patient's care. Provide recommendations for adjusting the treatment plan and suggest tasks or homework.
Finally, sign the ABA Session Notes, including your credentials, to confirm that the session was completed and approved. This signature validates the information recorded and ensures accountability in the treatment process.
Writing clear and concise session notes is crucial for data collection and effective communication among clinicians, tracking client progress, and substantiating billing claims. Documenting specific details about the client's progress, such as challenges and breakthroughs, is essential for a comprehensive view of their development. Here are some tips for writing effective ABA Session Notes:
When writing ABA Session Notes, describe the behaviors you observed. This level of detail helps therapists and caregivers understand exactly what occurred during the session, which is crucial for planning future interventions and tracking progress over time.
Using objective language means describing only what was directly observed without adding personal interpretations or judgments. This approach ensures accurate notes about what happened during the session, which helps maintain clarity and consistency in therapy records.
Include details about the environment where the session took place, such as noise levels, lighting, or any changes in routine. These factors can significantly impact behavior and provide important insights into why certain behaviors occur.
Link each observation in your notes to specific therapy goals or objectives. This practice helps demonstrate progress toward desired outcomes and allows therapists to assess whether current strategies are effective.
Write comprehensive notes by focusing on key behaviors and interventions that occurred during the session. Avoid lengthy descriptions or irrelevant details that can obscure important information. Clear and concise notes are easier to review and analyze, ensuring that therapists and caregivers can quickly grasp the session's outcomes and make informed decisions for future therapy sessions.